9.13. SOP for Event Based Surveillance
Standard Operating Procedure for Event Based Surveillance
Effective Date: 31st January
Version: 1.0
Prepared by: [Name/Department]
Approved by: [Name/Department]
1. Introduction
Event-Based Surveillance (EBS) is a critical component of the Integrated Disease Surveillance and Response (IDSR) system in Saint Lucia. It supplements indicator-based surveillance (IBS) by identifying signals from formal and informal sources to detect unusual health events or public health risks.
An early warning surveillance system is very important for early detection of outbreaks of diseases. A good surveillance system must be comprehensive and sensitive to achieve its objectives. Early warning and response (EWAR) should be an integral part of an existing public health surveillance and response system. It is designed to ensure the early detection of any abnormal / unusual occurrence of event so that the event may be verified and confirmed if applicable and measures for its control implemented in a timely manner. Therefore, Event-Based Surveillance (EBS) plays its role as one of the components within EWAR.
Event-Based Surveillance (EBS) constitutes an essential pillar of Saint Lucia's Integrated Disease Surveillance and Response (IDSR) system. EBS functions as an agile, supplementary mechanism to the traditional Indicator-Based Surveillance (IBS), facilitating the prompt detection of emerging health threats by capturing signals from both formal institutional channels and informal community-based sources.
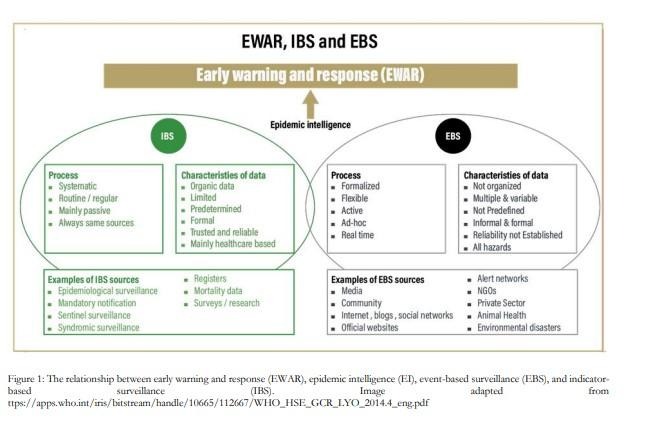
As a fundamental component of the Early Warning and Response (EWAR) architecture, EBS enables the timely recognition and management of anomalous health occurrences—events that may signal imminent public health crises. A robust surveillance system must exhibit both breadth and acuity, with EBS ensuring vigilance for deviations from normative health patterns, thereby safeguarding the public through expedited risk containment.
What is Event-Based Surveillance?
Event-based surveillance (EBS) is a method of rapidly collecting and analyzing information about health events and risks to provide early warning. EBS is used to monitor human, animal, and environmental health. These are usually unusual events occurring in the community which may have a known, suspected or possible impact on human health.
Event-Based Surveillance (EBS) is a dynamic approach to the rapid collection, assessment, and analysis of information related to potential public health threats. It serves as an early warning system by monitoring unusual occurrences across human, animal, and environmental domains that may pose actual, suspected, or potential risks to human health. EBS focuses on detecting atypical events within communities that fall outside established surveillance indicators but warrant prompt attention due to their possible health implications.
Purpose:
The purpose of this SOP is to outline the procedural framework for event-based surveillance in a comprehensive step by step manner to ensure timely detection, reporting, and response to events whilst defining the roles and responsibilities of all actors involved to ensure coordinated efforts.
Objectives:
- To rapidly detect and appropriately respond to acute public health events of any origin, ensuring timely implementation of effective control measures.
- To reduce the public health risk and impact of the events.
- To synergize EBS with existing indicator-based surveillance systems and other health intelligence platforms.
Scope:
This SOP is applicable to all public health actors in Saint Lucia, including healthcare providers, laboratories, environmental agencies, and other stakeholders involved in event-based surveillance activities.
Legal Framework:
Reference to national and international health regulations guiding event-based surveillance.
The procedures outlined herein are aligned with national legislation and international public health mandates, including the International Health Regulations (IHR 2005).
List legislation:
Sources of Event Information:
Information on events can be obtained from various sources:
- Within the healthcare system:
- Laboratories
- Primary and Secondary Healthcare facilities
- Mortality Registers
- Private practitioners
- Pharmacies
- Outside the healthcare system.
- Communities
- Other government or non-government agencies
- Media
- Police
- EMT responders
- Schools
- Regional and International agencies
2. Actors Involved and their Roles & Responsibilities
2.1 Epidemiology (Epi) Unit (Epidemiologist and Surveillance Officers)
- Role: This is the central body responsible for overseeing the entire surveillance process.
- Responsibilities:
- Develop national guidelines and protocols for event-based surveillance.
- Coordinate with regional health authorities including environmental health
- Provide training and resources to other health authorities including environmental health and other stakeholders.
- Analyse surveillance data and disseminate findings in a timely manner.
- Report outcomes to international bodies like the World Health Organization (WHO).
2.2 Environmental Health (EH)
- Role: The Environmental Health Unit central unit for receiving and verifying complaints.
- Responsibilities:
- Receive complaints.
- Preliminary investigation and verification of complaints in a timely manner.
- Update complaint information in DHIS2 platform (Epidemiology Unit to review) and provide all information as needed to the Epidemiology Unit
- Assess the complaint, and undertake the corrective measures to address the complaint as deemed necessary.
2.3 Healthcare Units
- Role: Healthcare units are responsible for the initial detection of some events
- Responsibilities:
- Prompt identification, documentation and reporting of unusual clinical patterns
- Notification of suspected clusters or events to the Epidemiology Unit
Components of the EBS System:
- Event detection:
- Detection is the process of capturing information through various modalities (e.g., in the community, healthcare workers, via media reports, etc.) on potential health events.
- To ensure the proper functioning of an EBS system, the community should be aware of:
- what to report
- who to report to
- where to report any event of concern.
- Key information on each event of concern should be collected and recorded in the DHIS2 EBS Module to facilitate the verification process.
- Event Triage:
- After detection, the information needs to go through a process of triage in order to assess relevance, eliminate duplication and retain only the information deemed pertinent to early detection purposes i.e. signals.
- A signal is any information about a potential health event that requires further verification. Questions to ask during the triage process include:
- Is the reported information relevant to early warning (i.e., could this signal be a genuine health threat?
- Was the signal previously reported (i.e., is the signal a duplicate?
- Information for the same event may be reported simultaneously from different sources or are reported repeatedly from the same source; this is usually an indication of the severity of the threat.
- The country priority event list (Annex 1) serves as a guide of whether or not information could signify a genuine health threat.
- Once information is triaged, it becomes a “signal”.
- Any signal that has the potential to be relevant to EWAR and is not a duplicate must then be verified.
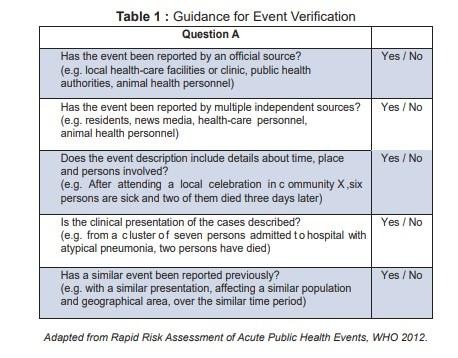
- Verification:
- The process by which a signal, can be substantiated, to confirm whether it is valid.
- Guidance for event verification can be found in Annex 2. Not all confirmed events, however, pose a potential risk to public health and guidance to determine the public health risk is found in Annex …
- All signals detected must be verified to become an event.
- Verification of a signal is usually performed at the local level nearest to the location of the signal.
- The purpose of verifying potential public health event or signals is to determine the first important measure in the response.
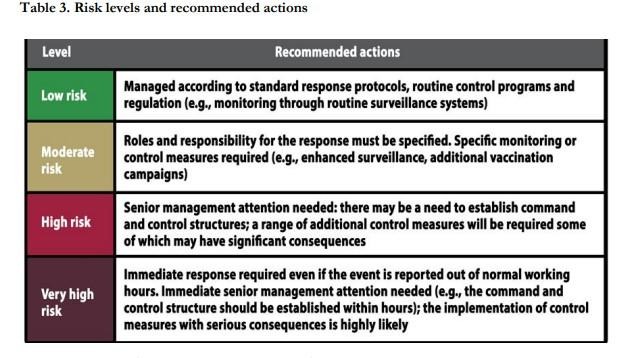
- Risk Assessment:
- Risk Assessment quantifies the threat level associated with a verified event, incorporating hazard characteristics, population vulnerability, and potential health impact
- A risk assessment should be conducted within the first 24 hours of signal verification (within 48 hours of signal detection) and should be repeated as new information becomes available until the end of the response to an event.
- The team must conduct (i) hazard (ii) exposure and (iii) context assessments in order to determine the level of risk, a process known as ‘risk characterization’. See algorithm below.
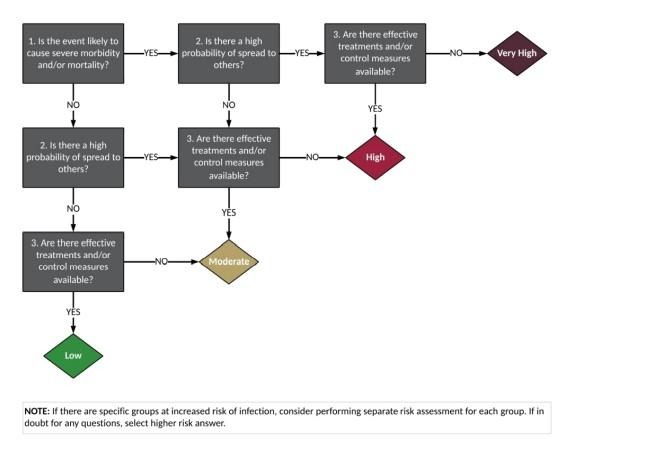
A more detailed risk assessment is given in Annex 3.
- Response, Communication & Feedback:
Based on the results of the assessment and risk characterization of potential threat by RRT, a response is formulated. See guidance below.
Surveillance Procedures
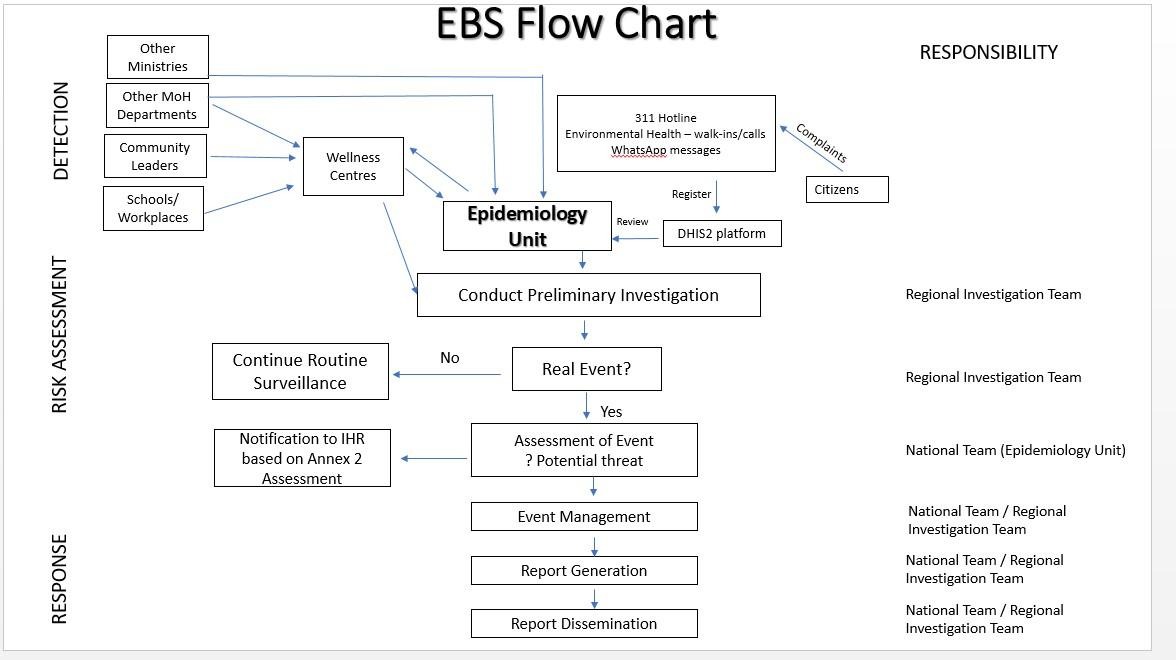
Flowchart – Events-based Surveillance
Step 1: Signal Detection and Triage:
Epi Unit
- Monitor signals originating from various formal and informal sources:
Healthcare Units
- Identify and report unusual events within 24 hours of detection to the Epidemiology Unit
- Report all unusual clusters of illnesses, sudden death or specific symptoms
Environmental Health
- Receive complaints from citizens (via hotlines / online source provided / walk-ins)
- Register complaints in the complaints DHIS2 platform
- If the complaint is not relevant to the unit, pass it along to relevant unit
- Once the complaint is relevant to unit, pass on to the person in charge of verification
- Verify complaint (add additional information to DHIS2 platform, assessable by the Epidemiology Unit)
- Assess the event and the action needed
- Initiate action as needed
- Report to Epi Unit as needed
311 Hotline/ WhatsApp
- Receive complaints from citizens (via hotlines / online source provided / walk-ins)
- Register complaints in the complaints DHIS2 platform
- Typically, both detection and triage occur at the same time with hotlines.
Step 2: Signal Verification and Testing– Regional Outbreak/Investigation Team)
2.1. Signal Verification –
- Verify the authenticity and relevance of the signal. Criteria for verification includes unusual occurrence or cluster; public health significance – severity, transmissibility (See Box 2 and Box 3 in the Annex for proposed list of signals to be reported by the community and non-health sector; by the One Health sector).
- Contact the source for additional information.
- Generate and submit report to Epidemiology Unit
Table 1: Proposed Action Post Event Verification
Step 3 – Risk Assessment (Epidemiology Unit)
- The risk assessment is done at the national level and will comprise of a team consisting of the following:
- National Epidemiologist/Medical surveillance Officer
- Environmental Health Officer (Vector control/ Food Unit/ Port Health/ Institutional hygiene unit based on the nature of the event.
- Public Health Nursing Supervisor
- Bureau of Health Promotion Officer
- District Medical Officer (if required)
- Other subject matter experts (such as Veterinary/Agricultural Officers) will be co-opted based on the nature of the event.
- Risk assessment helps prioritize which events require immediate action and which can be handled with less urgency.
- Risk Assessment involves evaluating the potential harm or threat posed by a detected event. It considers factors like the likelihood of the event occurring, magnitude, severity, and potential impact of the event, such as the number of cases or deaths, the severity of the illness, and the novelty of the event.
- Use risk assessment frameworks such as the WHO’s Rapid Risk Assessment tool (See Annex 3)
Step 4 - Investigation (Epidemiology Unit)
- The investigation is a more in-depth process than the risk assessment and aims to understand the specific details of the event, including the cause, scope, and potential sources.
- Investigations involve collecting data, interviewing individuals, conducting laboratory analysis, and implementing control measures to prevent further spread.
- The investigation team will comprise the same individuals as in Section 3.3.
Step 5: Data Management (Epidemiology Unit)
- Data should be cleaned and analysed
- A report should be completed after event verification, risk assessment and field investigations
- Dissemination of a periodic situation report may be necessary for ongoing threats.
Step 6: Response, Communication and Feedback
- Develop response plans based on the assessed risk, coordinating with healthcare facilities, laboratories, and other partners.
- Notify relevant authorities for significant events.
- Share updates internally (surveillance team and healthcare provider)
- Issue public advisories or press releases as deemed necessary (use multiple platforms to disseminate information – MoH webpage, via word of mouth through community nurses, bulletins in health facilities, What’s App groups)
- Provide timely feedback to reporting entities to encourage continuous participation.
MONITORING AND EVALUATION OF EVENT-BASED SURVEILLANCE
a) Signals and events reported
- Number of signals reported through EBS quarterly
- Number of signals verified through EBS quarterly
- Number of events assessed through EBS quarterly
- Number of events responded through EBS quarterly
b) Timeliness of reporting/response
- Time in hours from signal detection to event reporting to the district level
- Time in hours from signal detection to the response
Short-term outcomes:
- Signals detected and reported
- Events reported and responded
Intermediate outcomes:
- Time of notification and response
- High acceptance of EBS by implementers at each level
- Increased trust among the community
Long-term outcomes:
- Reduction of morbidity and mortality associated with infectious diseases
Annex 1: Proposed list of signals to be reported
Healthcare Facilities
- Severe illness requiring hospital admission in health care workers after caring for patients with similar symptoms
- Large, unexpected, sudden increases in admissions for any illness of the same type, including patients in intensive care units
- Severe, unusual, unexplainable illness including failure to respond to standard treatment
- An unusual pattern of disease in the community.
- An illness with signs/symptoms the community has not seen before.
- Two or more people presenting with similar symptoms with a history of recent travel, residing in the same community, school or workplace in the same seven-day period, especially:
- With high fever, stiff neck
- With high fever, yellow eyes or skin
- Cluster of deaths in a healthcare facility.
- A single case severe enough to require admission to hospital or causing death of any of the following:
- Three or more rice watery stools in 24 hours with dehydration (fatigue, thirst or sunken eyes)
- A respiratory infection with fever in someone who has been traveling abroad in the last 14 days
- Illness after contact with sick or dead animals
- Illness with fever, watery diarrhea and unexplained bleeding (gums, skin, or eyes, stool or urine)
Community
- Any child less than 15 years old:
- With sudden weakness of limb(s)
- With fever and skin rash
- Cluster of deaths in a village/community or facility
- Cluster of disease of unknown etiology in a village, community or facility over a 2-week period.
- Any unusual occurrence in the community which may affect human health.
- Any event that poses a risk to public health, including natural disasters, or symptoms / diseases rarely seen in the community
Animal Sector
- Severe illness in veterinarians, wildlife staff, or community members after contact (culling, feeding, treating, vaccinating) with a sick or dead animal
- Unexpected, sudden increases in disease or death of animals (including marine life)
- Sudden increase in abortions in animals
- All immediately notifiable zoonoses
Laboratories
- A pathogen that has not been detected for a long time in that country or a new pathogen
- Large/sudden unexpected increase in numbers of specimens with the same testing request, or positive result for the same pathogen (including the pathogens that are resistant to multiple antibiotics)
- Any pathogen on the immediately notifiable list
- Un-subtypeable or new influenza strain from a patient with Severe Acute Respiratory Infection (SARI)
Annex 2: Example of Indicators – Signal Reporting Form
Annex: 2
Annex: 3
POTENTIAL PUBLIC HEALTH RISK ASSESSMENT FOR EVENTS DETECTED
Examples for the application of the decision instrument for the assessment and notification of events that may constitute a public health concern.
(The examples appearing in this Annex are not binding and are for indicative guidance purposes to assist in the interpretation of the decision instrument criteria)
I. IS THE PUBLIC HEALTH IMPACT OF THE EVENT SERIOUS?
1. Is the number of cases and/or number of deaths for this type of event large for the given place, time or population?
2. Has the event the potential to have a high public health impact?
The following are examples of circumstances that contribute to high public health impact:
- Event caused by a pathogen with high potential to cause epidemic (infectiousness of the agent, high case fatality, multiple transmission routes or healthy carrier).
- Indication of treatment failure (new or emerging antibiotic resistance, vaccine failure, anti-dote resistance or failure).
- Event represents a significant public health risk even if no or very few human cases have yet been identified.
- Cases reported among health staff.
- The population at risk is especially vulnerable (refugees, low level of immunization, children, elderly, low immunity, undernourished, etc.).
- Concomitant factors that may hinder or delay the public health response (natural catastrophes, armed conflicts, unfavorable weather conditions, multiple foci in the State Party).
- Event in an area with high population density.
- Spread of toxic, infectious or otherwise hazardous materials that may be occurring naturally or otherwise that has contaminated or has the potential to contaminate a population and/or a large geographical area.
3. Is external assistance needed to detect, investigate, respond and control the current event, or prevent new cases?
The following are examples of when assistance may be required:
- Inadequate human, financial, material or technical resources – in particular:
- Insufficient laboratory or epidemiological capacity to investigate the event (equipment, personnel, financial resources);
- Insufficient antidotes, drugs and/or vaccine and/or protective equipment, decontamination equipment, or supportive equipment to cover estimated needs;
- Existing surveillance system is inadequate to detect new cases in a timely manner.
Is the public health impact of the event serious?
Answer “yes” if you have answered “yes” to questions 1, 2 or 3 above.
II. IS THE EVENT UNUSUAL OR UNEXPECTED?
4. Is the event unusual?
The following are examples of unusual events:
- The event is caused by an unknown agent or the source, vehicle, route of transmission is unusual or unknown.
- Evolution of cases more severe than expected (including morbidity or case- fatality) or with unusual symptoms.
- Occurrence of the event itself unusual for the area, season or population.
5. Is the event unexpected from a public health perspective?
The following are examples of unexpected events:
- Event caused by a disease/agent that had already been eliminated or eradicated from the State Party or not previously reported.
Is the event unusual or unexpected?
Answer “yes” if you have answered “yes” to questions 4 or 5 above.
III. IS THERE A SIGNIFICANT RISK OF SPREAD?
6. Is there evidence of an epidemiological link to similar events in other districts / states/ country?
7. Is there any factor that should alert us to the potential for cross border movement of the agent, vehicle or host?
The following are examples of circumstances that may predispose to spread:
- Where there is evidence of local spread, an index case (or other linked cases) with a history within the previous month of:
- Recent travel; local / international (or time equivalent to the incubation period if the pathogen is known);
- Participation in a gathering; local / international (pilgrimage, sports event, conference, etc.); Close contact with a traveler or a highly mobile population.
- Event caused by an environmental contamination that has the potential to spread across borders.
- Event in an area of intense traffic with limited capacity for sanitary control or environmental detection or decontamination.
Is there a significant risk of spread?
Answer “yes” if you have answered “yes” to questions 6 or 7 above.
IV. IS THERE A SIGNIFICANT RISK OF TRAVEL OR TRADE RESTRICTIONS?
8. Have similar events in the past resulted in restriction on trade and/or travel?
9. Is the source suspected or known to be a food product, water or any other goods that might be contaminated that has been exported/ imported to/from other districts / states / country?
10. Has the event occurred in association with a gathering or in an area of intense tourism?
11. Has the event caused requests for more information by officials or media?
Is there a significant risk of trade or travel restrictions?
Answer “yes” if you have answered “yes” to questions 8, 9, 10 or 11 above. (Note: Adapted from Annex 2, IHR 2005)
Key steps for conducting rapid risk assessment are:
- The EBS FP at the intermediate level (e.g., District medical officer) convenes a multi-disciplinary team.
- The team then conducts rapid risk assessment, based on pre-defined risk questions, by considering Hazard, Exposure and Context.
Hazard Assessment
This refers to the identification of the characteristics of a health hazard and the associated health threat. Hazards include biological, chemical, radiological, physical, and nuclear events. The assessment process includes:
Use available clinical and epidemiological features for laboratory confirmed agents, when available. In all other cases, start with listing possible causes based on:
- The initial description of the event.
- Known burden of diseases in the affected community; and
- Type and distribution of existing hazards (e.g., the number and location of chemical plants and the chemicals they use).
Possible questions to ask:
- Is this threat unusual or unexpected?
- Is this event new in the country?
- Is this occurring in an unusual or unexpected setting, mode of transmission, and/or population group?
- Are there novel clinical manifestations that result in severe illness, disability, and/or death?
- Is the threat likely to cause severe disease in this population/group?
Considering the pathogen, exposed population, and availability of treatment where the event is occurring, will more than 20% of people infected develop severe illness, severe disability, and/or die?
Exposure Assessment
This refers to the evaluation of the exposure of individuals and populations to likely hazards. The key output of the assessment is an estimate of the: (a) number of people or groups known or likely to have been exposed, and (b) number of exposed people or groups who are likely to be susceptible (not immune).
Information required to evaluate exposure includes:
- Mode of transmission/exposure (e.g., direct contact, droplet, sexual, occupational).
- Incubation period (known or suspected).
- Estimation of the potential for transmission (e.g., R0 basic reproduction number); Immune status of the exposed population.
- Disease burden in and distribution of vector or animal hosts/reservoirs for vector-borne and zoonotic diseases.
- Dose (e.g., amount ingested/absorbed/inhaled) and duration of exposure
Possible questions to ask:
- What is the probability of spread beyond the location of occurrence?
- Is exposure geographically widespread or limited to specific sub-groups (e.g., immunodeficient, comorbidities, socially/economically vulnerable, location)?
- Does infection/exposure occur from a low dose?
- Is this readily transmitted person-to-person (e.g., by airborne)?
- If an animal event, is there a potential for the pathogen to spread from animals to humans?
- Are treatment or prevention measures available for animals or people?
- Does the event/pathogen cause severe morbidity or mortality in humans?
- Does the agent have the potential for person-to-person transmission?
Context Assessment
This refers to the evaluation of the environment in which the event is taking place. This may include:
- The physical environment such as climate, vegetation, land use (e.g., farming, industry) and water systems/sources
- Health of the population (e.g., nutritional status, disease burden and previous outbreaks),
- Infrastructure (e.g., transport links, healthcare, public health 19 infrastructure),
- Cultural practices and beliefs and/or
- Political environment (civil wars, terrorist attacks)
Context assessment should consider all factors that can affect the risk level of the event including social, ethical, technical, scientific, economic, environmental, and political. For example:
- For measles, outbreak spread depends upon factors like the current immunisation coverage in the population, the capacity to quickly organise mass vaccination campaigns if coverage is low, general hygiene and access to health care, the MS surveillance capacity to rapidly detect and isolate cases, and population movement and behaviour.
- For water contamination events by chemical agent, the risk of human intoxication will depend on factors like local water use practices, seasonality (cold or hot, rainy, or dry), the flow of the water source, capacity to quickly broadcast risk and prevention messages to the public, and public acceptability of control measures.
Possible questions to ask:
- Are effective treatments and control measures available in the Member State?
- Even if treatment and control measures exist somewhere in the world, answer “no” if they are not immediately and widely available in the specific setting where the event is occurring.
- Is there an ongoing socio-political crisis that could hinder mobilisation of resources or possible interventions?
- Are the affected areas accessible to responders? (Free of hostility) Risk characterization
Once the EBS unit has carried out the hazard, exposure, and context assessments, a level of risk should be assigned. This process is called risk characterization.