9.16. Leptospirosis
Standard Operating Procedure for the Integrated Surveillance of Leptospirosis
Effective Date: [Date]
Version: 1.0
Prepared by: [Name/Department]
Approved by: [Name/Department]
1. Introduction
- Purpose:
The purpose of this standard operating procedure (SOP) is to outline the procedures for the integrated surveillance of leptospirosis in a comprehensive step by step manner to ensure timely detection, reporting, and response to outbreaks. It defines the roles and responsibilities of all involved actors to ensure coordinated efforts. - Scope:
This SOP applies to all public health entities, healthcare providers, animal health officials, laboratories, and other stakeholders involved in leptospirosis surveillance. - Definitions:
- Leptospirosis: An infectious zoonotic disease caused by pathogenic bacteria called leptospires, that are transmitted directly or indirectly from animals to humans, with very rare human-to-human transmission.
- Surveillance: Systematic collection, analysis, and interpretation of health data.
- Legal Framework:
Reference to regional/international health regulations guiding the surveillance and control of leptospirosis.
2. Actors Involved and Their Roles
2.1 Epidemiology (Epi) Unit
- Role:
- This is the central body responsible for overseeing the entire surveillance process for human health.
- Responsibilities:
- Develop national guidelines and protocols for leptospirosis surveillance.
- Coordinate with the Ministry of Agriculture/ Animal or Livestock Health unit, Environmental Health, regional health authorities, and laboratories.
- To collaborate with the named national actors on the investigation of leptospirosis outbreaks/cases, and implementation of outbreak response measures, and prevention and control measures utilising a One Health approach.
- Provide training and resources on integrated surveillance to the prioritized units, healthcare providers and other stakeholders.
- Analyse surveillance data and disseminate findings.
- Provide timely and complete reporting of cases to regional and international bodies like the Caribbean Public Health Agency (CARPHA) and PAHO/WHO.
2.2 Veterinary Public Health/ Animal Health Unit
- Role:
The Veterinary Public Health/Animal Health Unit reports directly to the Chief Veterinary Officer and is responsible for the complete reporting, and investigation of outbreaks of and routine surveillance of leptospirosis in livestock, companion animals, wildlife, and rodents/pests. - Responsibilities:
- Utilise national leptospirosis surveillance guidelines
- Aid in the investigation and reporting of farms/districts who have reported leptospirosis outbreaks.
- Collaborate with the Ministry of Health Epidemiology Unit in prevention and control measures, and other mitigation measures surrounding the transmission of leptospirosis.
- Submit relevant surveillance data to the Epidemiology Unit.
- Conduct passive and active surveillance for leptospirosis in livestock and companion animals.
- Submit serovar surveillance findings for leptospirosis in livestock and companion animals to the Epidemiology Unit.
2.3 Health Units (HU)
- Role:
The HU is the frontline body responsible for detecting and managing leptospirosis cases within the community. - Responsibilities:
- Conduct passive surveillance of leptospirosis.
- Assist the Epidemiology Unit in the response
- Ensure timely reporting of suspected cases to the Epidemiology unit.
- Engage in public health education and community outreach.
- Take samples of people suspected to have leptospirosis and ship to the national laboratory following national guidelines for shipping of samples.
- Check with laboratory for results
- Inform persons of their test results.
2.4 Healthcare Providers (HCPs)
- Role:
Healthcare providers are responsible for the initial detection and clinical management of mpox cases. - Responsibilities:
- Identify and report suspected cases of mpox to health units.
- Collect and submit clinical samples for laboratory testing.
- Provide clinical care to patients according to national guidelines.
- Educate persons with mpox and those that accompany them about mpox prevention and control.
2.5 Laboratories
- Role:
Laboratories play a crucial role in the confirmation of mpox cases. - Responsibilities:
- Provide instructions for sample collection and packaging in accordance with applicable guidelines.
- Receive samples and laboratory form; inform the relevant unit about rejection of sample as necessary.
- Conduct diagnostic testing for mpox.
- Report laboratory results to healthcare providers and health units according to established reporting channels.
- Maintain quality controls in testing procedures.
- Share data with Epi and STI Unit and collaborate on epidemiological studies.
- Training on collection, conservation of samples and transportation.
2.6 Surveillance at Point of Entry
- The immigration officers must share the Health Alert Notice card containing information to all travelers
3. Surveillance Procedures
Step 1: Case Detection – Healthcare Providers / Laboratory Personnel
1. Immediate Reporting: Report all confirmed cases to the Epidemiology Unit and Environmental Health Department immediately for follow up. (Case definitions below)
Suspected leptospirosis case definition
Evocative epidemiological context; and clinical signs and symptoms consistent with leptospirosis:
- abrupt onset of fever
- chills
- conjunctival suffusion
- headache
- myalgia
- jaundice
- cardiac or renal failure
- and pulmonary haemorrhage.
Probable leptospirosis case definition
A suspected case and the presence of Leptospira immunoglobulins type M (IgM) in one serum sample detected by serology (e.g. Immunoglobulin M (IgM) enzyme-linked immunosorbent assay (ELISA)).
Confirmed leptospirosis case definition
A suspected case confirmed by laboratory test as follows:
- seroconversion or a four-fold or higher rise in titre detected by serological techniques (e.g. microscope agglutination technique (MAT) or IgM ELISA) in consecutive serum samples; or
- detection of Leptospira DNA from a clinical specimen by polymerase chain reaction (PCR); or
- demonstration of Leptospira spp. in tissue
2. Conduct Epidemiological Investigation with Environmental Health/Epidemiology Unit to prevent the spread of disease
- Use personal protective equipment for the management of cases in isolation
- In the case of institutional isolation, this can be done after the opinion and evaluation of the care provider
- In the case of community isolation, it is advisable to wait until the rash has fully healed and a fresh layer of skin has formed
- All case records except demographic information and HIV/STI status must be available and shared with STI and Epi Unit; this is to better organize investigations, prevent leaks and facilitate feedback to the health institution or people directly concerned.
- Relevant demographic information and HIV/STI status will be shared only on a need-to-know basis.
3. Testing
Methods for collecting, preserving and transporting specimens-
Presumptive diagnosis
- A positive result of a rapid screening test such as IgM ELISA, latex agglutination test, lateral flow, dipstick, etc.
Confirmatory diagnosis
- Isolation from clinical specimen (blood, urine, CSF or tissue) through culture of pathogenic leptospires.
- A positive PCR result using a validated method (primarily for blood and serum in the early stages of infection).
- Fourfold or greater rise in titre or seroconversion in microscopic agglutination test (MAT) on paired samples obtained at least 2 weeks apart. A battery of Leptospira reference strains representative of local strains should be used as antigens in MAT.
Specimen Collection and Transport
- Acute blood, urine, CSF or tissue
- Specimens for isolation of Leptospira should be transported to the laboratory at ambient temperature within 24 hours.
- Urine specimens may be taken 10 days after the onset of illness for Leptospira isolation. Other specimens should be taken as soon as the patient is seen.
- Blood for ELISA IgM
- This should be collected when the patient is seen and transported to the laboratory at 4 oC within 24 hours. Only one specimen is needed for ELISA IgM titre. If the result falls in the uncertain category, then a second sample is requested.
- Convalescent blood specimen
- A second blood sample should be collected at least 2 weeks after the first and transported to the laboratory at 4 oC within 24 hours.
Specimen submission
Specimens must be properly sealed and labelled and accompanied by the following minimum information- name of patient, address, date of onset, date of specimen, occupation of patient and history of animal contact.
3. Treat clients according to national guidelines
Step 2 – Epidemiological Investigation
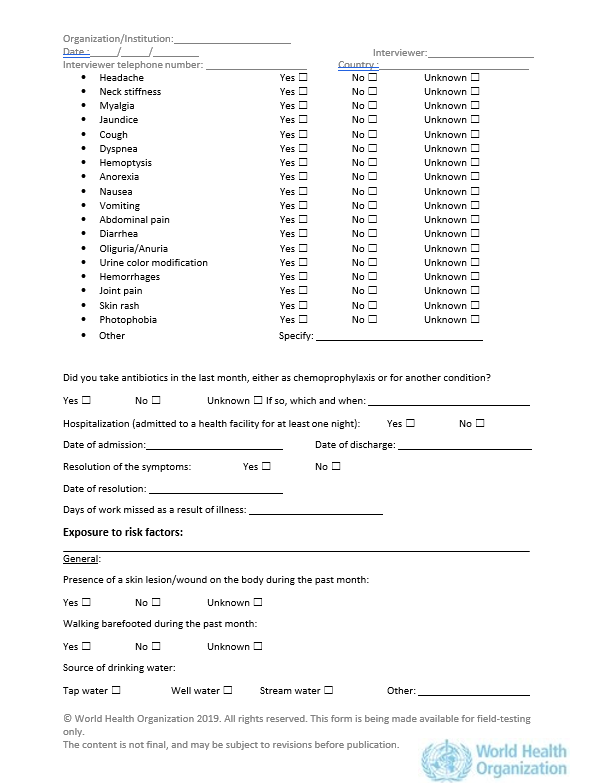
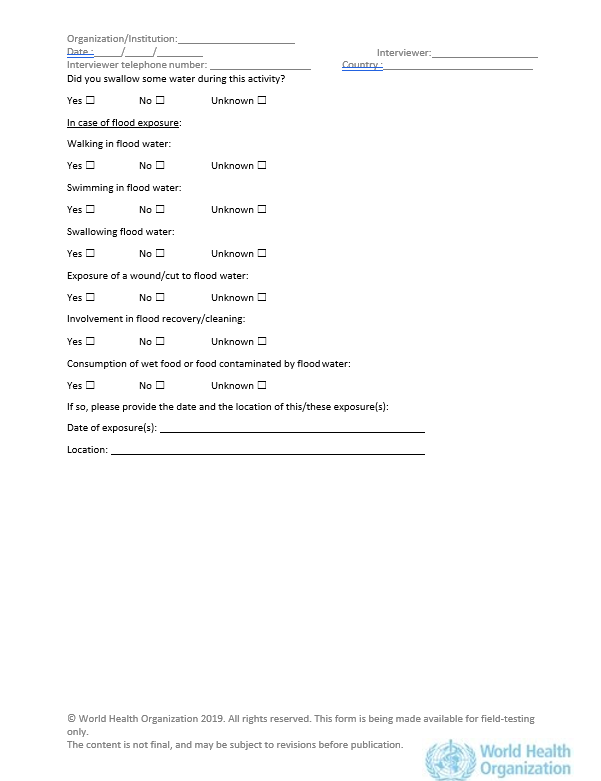
- Complete the reporting form handed over from the Healthcare Provider as required (at the end of the document).
- Conduct an investigation
An investigation team may be made up of :
- 1 or 2 trained staff from the Epidemiology Unit
- 1 or 2 staff from the Environmental Health Department
- 1 surveillance nurse or medical technologist
- 1 trained staff from Veterinary Public Health
The investigation should entail :
- Case should be interviewed to verify the date of onset of symptoms and to identify possible exposure scenarios.
- Review possible exposures.
- Confirm the test results with the public health laboratory.
- Contact Animal Health/Veterinary Public Health to review animal sources of exposure.
- Review climatology/meteorology reports to note if exposure linked to increased rainfall and associated flood events.
- Site visits to animal farms/abattoirs should be conducted by Veterinary Public Health as needed.
- Site visits to food establishments/ manufacturing plants, etcetera conducted by Environmental Health Department for occupational exposure.
- Contact tracing to identify other individuals at risk of infection.
- Conduct interviews on sites to identify other clincally compatible cases for follow up.
- Implement control measures.
Deliverables of the investigation team :
Investigation of suspected cases
- Completion of the investigation form
- Identification of contacts and samples to be taken from contacts which fulfils the suspected case definition
- Collection, conservation and transport of specimens
- Submit the investigation forms to relevant entities.
Contact tracing
- Locate and follow up on contacts (home visit, telephone follow-up)
- Preliminary assessment of each contact
- Samples to be taken from contacts which fulfils the suspected case definition
- Collection, conservation and transport of specimens
- Submit information collected to relevant entities
3. Control and Prevention Strategies
Step 3: Data Management (STI and Epi Unit)
- Data should be cleaned and analysed
- Preparation of a report should be done on the evolution of the epidemiological situation of the disease
- Dissemination of a weekly situation report
Indicators for monitoring the quality of mpox surveillance include:
- Proportion of suspected cases for which laboratory tests were carried out.
- Proportion of probable and confirmed cases with complete information on clinical and risk factors.
- Proportion of suspected cases for which test results are available within 24 hours of sample being taken.
Leptospirosis Case Reporting Form / Case Investigation Form
Case investigation form: PDF | Word